Fever In Children

Contents:
- What it a Fever?
- Why Do Children Have Fever?
- Fever Types
- Symptoms if a Fever
- Complications and Consequences
- Diagnostics and Examinations
- Fever Treatment
- Fever Prevention
Fever in Babies
Baby fever actually is a defensive reaction of a body, which happens in response to progressing of various infection diseases or due to pathologies of non-infectious genesis. Sometimes a fever appears in a form of physical condition that doesn’t require special treatment.
What it a Fever?
Fever (heat, hyperthermia) is a body’s reaction: body temperature raises because pyrogens affect thermoregulatory center. An increase in temperature has a protective character. When a fever is moderate, the production of body’s own interferons and other substances, badly affecting bacterial and viral agents, increases. Moreover, temperature’s increase affect bacteria and viruses too, reducing their ability to reproduce.
To diagnose a fever you have to know what temperature is considered normal for a child:
- if baby is less than 3 months old, its normal temperature is one up to 37.5 °C;
- if baby is less than 5 years old, its normal temperature is one up to 37.1 °C;
- if baby is older than 6 years, its normal temperature is between 36.6-36.8 °C.
Rectal and oral temperature is always higher than auxiliary and inguinal one, and is between 37-37.2 °C approximately.
Why Do Children Have Fever?
Many children’s diseases are followed by a fever. All hyperthermia causes can be divided in two groups: infectious and non-infectious. Infectious causes of a fever are: viral, bacterial, chlamydial, mycoplasma, parasitic (salmonellosis, enterobiosis), fungal and intestinal infections. Various infectious diseases (whooping cough, rubella, measles, chicken pox) are often followed by a fever.
Some infectious pathologies have specific names, such as Ebola, hemorrhagic, yellow, three-day, rat fever and others. Only some infections aren’t followed by a temperature’s increase: ones like botulism and cholera. Fever also follows inflammatory processes happening in internal organs (bronchitis, pneumonia, meningitis, meningoencephalitis), in mucous membranes (stomatitis, sore throat) and in skin (erysipelas). Temperature’s increase of non-infectious genesis rarely exceeds 38-38.5 °C.
The most common non-infectious causes of a fever are:
- allergy;
- rheumatism;
- teething;
- immune disorders;
- oncological and hematological diseases;
- endocrine disorders;
- poisoning;
- insect bites;
- heredity;
- iron-deficiency anemia;
- hyperactivity;
- obesity;
- traumas;
- intake of some medications.
Moreover, fever in babies can be caused by vaccination, by prolonged exposure to the sun or by stress. Sometimes the fever isn’t based on something serious and is just physiological. Babies have transitory fever during the period of active growth. Infants may suffer from fever on 3-5 day of their lives: this matches with the peak of their physiological weight loss.
If fever’s cause is impossible to identify and there are no evident symptoms of infectious or non-infectious diseases, this is called a fever of unknown origin. Sometimes this means that baby has autoimmune pathologies, or that neoplastic processes take place in baby’s body, or that ordinary disease progresses atypically.
Fever Types
Fever is measured by stages of temperature’s increase and can be:
- subfebrile – up to 37.9 °C;
- febrile – up to 38.9 °C;
- paretic – up to 40.9 °C;
- hyperparetic – above 41 °C.
By duration fevers can be:
- sharp – up to 15 days;
- subacute – up to 45 days;
- chronic – longer than 45 days.
Fevers can also differ basing on the fluctuations of body temperature during the day and can be:
- constant: fluctuations are within 1 °C, the temperature remains high for a few days in a row (typhus fever, lobar pneumonia);
- intermittent: normal temperature alternates with hyperthermia every 1-3 days (malaria);
- remittent: it may waver in 1-2 °C during the day, but still doesn’t drop to normal range (purulent diseases);
- hectic: fluctuations above 3 °C every few hours, sharp rise and fall of a temperature (septic conditions);
- wavy: temperature increases and lowers gradually (Hodgkin's disease, brucellosis);
- recurrent: the temperature rises to 39-40 °C periodically, followed by subfebrility (relapsing fever);
- wrong: has no definite pattern (rheumatism, cancer pathology, flu, pneumonia);
- warped: body temperature is higher in the morning than in the evening (sepsis, viral diseases, tuberculosis).
Symptoms of a Fever
A fever itself is a symptom. However, its symptoms may differ depending on a type of a fever.
If a fever is white, pale or cold, baby suffers from:
- paleness of a skin and mucous membranes;
- rapid breathing;
- slackness and chills.
The skin is moist and cool to the touch due to the vascular spasm. The limbs are icy.
Pink fever has the following symptoms:
- skin is warm, moist and flushed;
- limbs are warm;
- baby’s health is satisfactory.
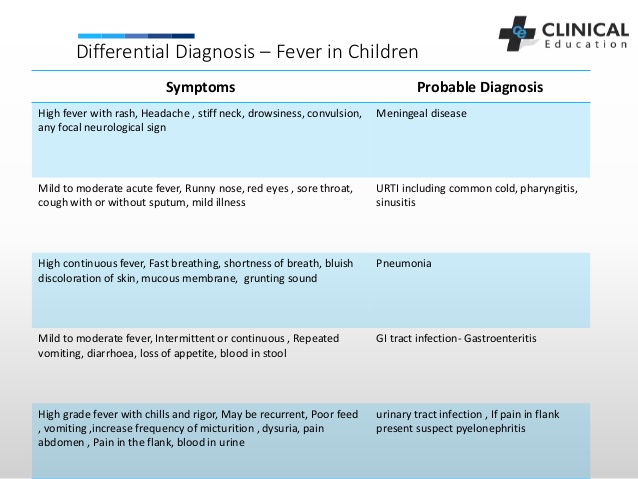
If a baby suffers from various illnesses, a fever can be followed by other symptoms, which allow differentiating a pathology correctly. Let’s talk more about some diseases that have fever as a primary symptom.
Complications and Consequences
One of the most common complications of fever in babies of small age (up to 5 years) are febrile convulsions. Strong fever can lead to lethal consequences without operational assistance.
Diagnostics and Examinations
If a temperature is high, you should contact a pediatrician immediately or to call an ambulance. After initial examination a doctor can prescribe you additional consultations of various specialists (surgeon, infectious disease specialist, allergist, ENT, etc.). The algorithm of examination depends on a type of a fever, on following symptoms and on baby’s condition.
Such tests are obligatory in case of hyperthermia:
- general urine and blood tests;
- X-ray examination.
Further diagnosis in conducted by more narrow specialist and may include various tests (kidney ultrasound, bacteriological and serological tests, rheumatic samples, electroencephalography and others).
Fever Treatment

To fight fever you have to start with treating the main disease that caused it. Depending on a cause, doctor can prescribe antivirals or antibiotics to a baby. Physic cooling and antipyretics are the basics of symptomatic treatment. You can try lowering the temperature only after it reaches 38.5 °C. If a baby is prone to febrile convulsions, you can try lowering the temperature when it reaches 37.9-38 °C.
First, you have to try lowering the temperature with the help of physical methods:
- put cool compresses on baby’s forehead, on the axillary and inguinal area;
- wipe a baby with weak vinegar liquor of with 40 % alcohol.
If physical methods don’t help, a doctor has to prescribe antipyretics to a baby.
Pediatricians are allowed to prescribe the following antipyretic medicine:
- Paracetamol (Panadol);
- Ibuprofen (Nurofen) – but with some restrictions.
You shouldn’t give the following medicine to the babies:
- Analgene: until your child is 12 or in case it is strictly prescribed by a doctor;
- Ibuprofen: if a baby has peptic ulcer or asthma;
- Aspirin: until your child is 15.
How to take antipyretics:
- they can be taken 3-4 times a day maximum;
- a baby shouldn’t take them for more than 3 days in a row or for high temperature’s prevention;
- it is better to alternate several antipyretics with a different active component during the day (for example, Panadol with Nurofen);
- if a baby is small, it is better to give them antipyretics in form of suppositories.
If a baby has a pink fever and needs immediate emergency help, you have to:
- undress a baby completely;
- remove a diaper;
- wipe a baby with a damp towel;
- turn on a ventilator or a conditioner until ambulance arrives.
If you are treating white fever, you should combine antipyretics and physical cooling with energetic warming of baby’s limbs (this needs to be done in order to restore microcirculation).
Fever Prevention
It’s impossible to exclude the possibility of fever completely.
To reduce the risk of disease, you have to:
- stick to the sanitary-epidemiological regime;
- monitor the baby’s hygiene;
- strengthen baby’s immunity;
- avoid hypothermia and hyperthermia.