Sudden Infant Death Syndrome (SIDS)
Contents:
- What Is SIDS?
- Causes Of Sudden Infant Death Syndrome
- Abortion Syndrome Of Sudden Infant Death
- Assessment Of The Risk Of Sudden Infant Death Syndrome
- Prevention Of Sudden Infant Death Syndrome
What Is SIDS?
Sudden infant death syndrome (SIDS, cot death, sudden infant death syndrome) is the unexplained death of an infant in a dream in the absence of adequate reasons, resulting in death. As follows from the definition, sudden infant death syndrome excludes the presence at the time of the death of infection, accident, not previously identified congenital (including genetic) or acquired diseases or their consequences. Not the study of the medical records of the deceased child, nor the view of place of death nor the autopsy results do not allow you to name a reason to explain the death.
The incidence of sudden infant death syndrome in the world is -0,2-1,5 cases (in Russia -0.43 cases) on 1000 children. At greater risk of SIDS exposed infants under the age of 8 months; the largest number of sudden deaths are of age 2-4 months. 60% of the children who died as a result of SIDS, are boys. Typically, the sudden death of a child occurs in the interval from midnight to 6:00 of the morning, mainly in winter. The proportion of sudden infant death syndrome accounts for up to 30 per cent of deaths among children in the first year of life, which explains the continued concern of young parents and specialists in paediatrics.
Causes Of Sudden Infant Death Syndrome

A study on the problem of sudden infant death syndrome has been ongoing for several decades, but a definite explanation of this phenomenon has not been received. To theories that represent historical interest include the explanation of the mechanism of sudden infant death syndrome by accident (random) shortness of breath (if a baby is in the parent’s bed, unintentionally smothering), squeezing the trachea enlarged thymus (asthma thymicum), lymphatic-hypo-plastic diathesis (thymico-status lymphaticus).
At the present stage in Child Neurology sudden infant death syndrome relates to sleep disorders (parasomnia). As one hypothesis explaining the pathogenesis of sudden infant death syndrome, sleep apnea is considered. Children with an increased risk of developing sleep apnea include premature babies with immature respiratory system.
Experience, accumulated by cardiology, indicates that among the causes of sudden cardiac death leading role belongs to violations of heart rhythm (arrhythmias). A large-scale study, which lasted for 20 years, found that the presence of according to ECG elongated QT interval increases the risk of sudden infant death at 41 times. A practical consequence of this opening served as ECG screening of newborns in some countries as a result of which children with congenital syndrome elongated QT-interval and an increased risk of SIDS are assigned to beta blockers.
One hypothesis to explain sudden infant death syndrome, serves as a suggestion that the situation of a sleeping child on his stomach with a head rotated on its side causes the compression of the vertebral artery, reduction of the brain stem perfusion and death of central apnea. The authors of this hypothesis propose as a screening method to identify children at risk of sudden infant death syndrome to use USDG of extracranial vessels.
Theory of violation of reactions of awakening and the ineffectiveness of the “catching” breath in response to hypoxia and hypercapnia growing in a child does not find a definite explanation. Perhaps the answer to sudden infant death syndrome lies in violation of sleep regulation, breathing and temperature homeostasis by neurotransmitter serotonin.
Supporters of other hypotheses attempt to explain sudden infant death syndrome pathogenesis by excess of endorphins, defects in beta oxidation of fatty acids, the lack of maturity of the cardio-respiratory control functions of the central nervous system, etc. Some authors suggest to attribute sudden infant death syndrome to the extreme manifestation of frontier conditions of newborns and babies in the first year of life, which may occur when exposed to a minimum of nonspecific factors by its expressiveness.
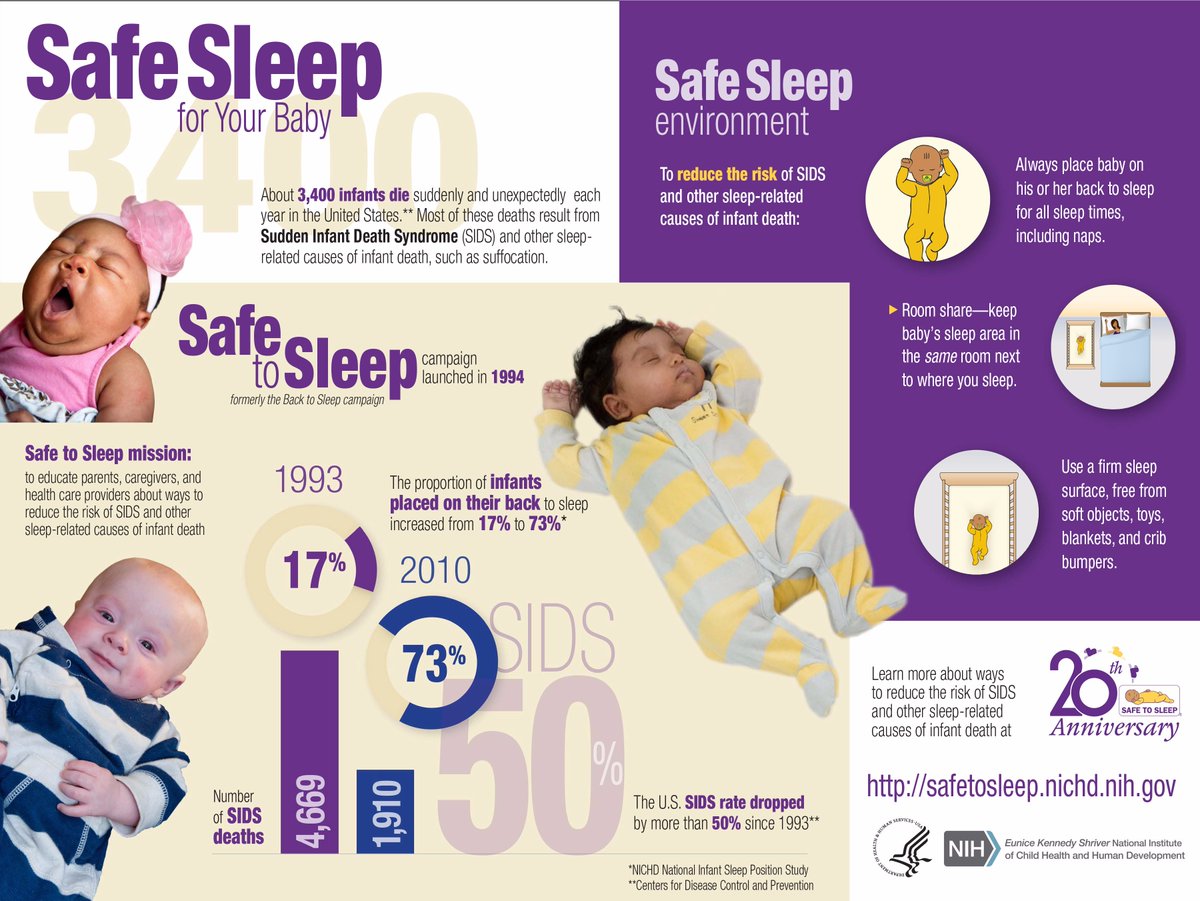
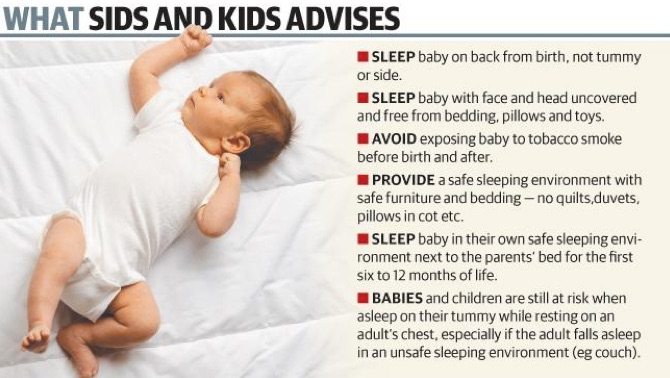
Despite the many hypotheses, none of which can serve as a generic explanation of the phenomenon of sudden infant death syndrome. However, perennial observations allow to identify a number of factors that significantly increased the risks of sudden infant death syndrome in infants. These include: young maternal age (under 20 years), multiple pregnancy, preterm labour, preterm child and weight less than 2500 grams, male baby, bottle-feeding, sleeping on my stomach and on a soft surface, overheating during sleep, smoking in the house, etc.
With respect to whether the risk of sudden infant death syndrome increases if a child is sleeping in the same bed with the parents, there is no unequivocal answer. Most researchers tend to see in a joint sleep preventing factor of sudden infant death syndrome due to synchronization of breathing and the heartbeat of the child with the breathing and heartbeat of the mother, as well as the ability of the mother to respond quickly to a stop of breathing in a child. On the other hand, the probability of sudden infant death syndrome increases because of excessive blanketing and overheating the child sleeping on a soft pillow, etc.
Contrary to misconceptions, preventive vaccination of children is not the cause of sudden infant death syndrome.
Abortion Syndrome Of Sudden Infant Death
With respect to infants who have experienced during infancy obvious life-threatening episode and have survived, the notion of abortive sudden infant death syndrome or near-miss SIDS is used. Typical signs of obvious life-threatening episode are sudden stops of breathing, pale or cyanotic skin color, hypotension or muscle hypertonia, arising in a child for no apparent reason, in full prosperity. Obvious life-threatening episodes during the first months of life arise in 0.6% of babies.
In 50-70% of cases of such children it is possible to reveal an obvious correlation of life-threatening episode with any pathological condition: convulsive syndrome, myopathy, infections of the respiratory tract, gastroesophageal reflux disease, congenital abnormalities, metabolic diseases, etc. Therefore, children who have suffered abortive sudden infant death syndrome, it is necessary to conduct a comprehensive survey with the participation of various children’s specialists: pediatrician, children’s neurologist, children’s cardiologist, children’s gastroenterologist, children’s pulmonologist, children’s otolaryngologist etc. Instrumental studies of the highest diagnostic value may be of EEG polysomnography, transcranial ultrasonic dopplerography, ECG, ultrasound of the heart child, Holter monitoring of ECG, chest x-ray. Laboratory techniques may include infectious diseases diagnosis (EIA, PCR, microbiological examination), biochemical analysis of blood, etc.
Assessment Of The Risk Of Sudden Infant Death Syndrome
The lack of reliable knowledge about the causes of sudden infant death syndrome allows to assess the risk solely by statistical methods. So to identify children at-risk groups is offered a Magdeburg table of SIDS points that highlights the criteria for the age of a mother, baby weight at birth, the position of the child in a sleep, especially bedding, smoking of a mother, breastfeeding duration.
Among the objective methods of singling out children groups at risk for development of sudden infant death syndrome to the forefront comes ECG and polysomnography.
The algorithm proposed by I.A. Kelmanson, contains 6 clinical and 12 morphological features, allowing for the postmortem differential diagnosis of a sudden infant death syndrome and life-threatening diseases and is of interest mainly for pathologists.
Prevention Of Sudden Infant Death Syndrome
When an apparent life-threatening episode you want to take the child on your hands, bother him, vigorously massaging the hands, feet, earlobes, back along the spine. These actions usually are enough for a kid to start breathing again. If breathing is not restored, there is an urgent need to call an ambulance and begin conducting artificial respiration and heart massage.
Sudden infant death syndrome prevention includes primary and secondary measures. Principles of primary prevention are based on antenatal interventions (refusal from harmful habits before pregnancy, the mother’s nutrition management, sufficient physical activity and the prevention of preterm birth, early registration and maintenance of pregnancy under the supervision of an obstetrician-gynecologist, etc.). Measures of primary prevention of sudden infant death syndrome also include optimization of conditions for sleeping of a baby: sleep on the back, use of sleeping bag, excluding independent revolution of a baby on a tummy, sleep on thick mattress, exclusion of overheating, adequate fresh air, maintaining adequate temperature and moisture, no sharp smells and tobacco smoke.
Secondary prevention of sudden infant death syndrome involves the identification of high-risk groups and carrying out targeted activities (tonic treatment, massage), a home cardiorespiratory monitoring, etc.
Video: What You Need To Know About SIDS