Postpartum Bleeding

Contents:
How Long Should Postpartum Bleeding Last
Postpartum bleeding is the bleeding from maternal passages arising in early or in the late postnatal period. Postpartum bleeding is most often an outcome indicator of the main obstetric complication. The severity of postpartum bleeding is determined by the blood loss.
Bleeding is diagnosed during examination of the maternal passages, inspection of the uterine cavity, ultrasonic scanning examination. Treatment of postpartum bleeding demands that infusion and transfusion therapy should be conducted. Uterotonic drugs are administered and tearings are sewn up. Sometimes a uterus extirpation has to be performed.
Postpartum Bleeding
Danger of postpartum bleeding is that it can lead to intensive loss of large volume of blood and death of the woman in labor. Heavy bleeding is promoted by intensive uterine blood flow and a big wound surface after the delivery. In normal conditions the organism of a pregnant woman is ready to physiologically admissible loss of blood in labor (up to 0,5% of body weight) due to increase in intra vascular volume of blood.
Besides, postpartum bleeding from the uterine wound can be prevented by the strengthened muscular contractions of the uterus, compression of uterine arteries and their shift in deeper muscular layers with simultaneous activation of blood coagulation and thrombi formation in small blood vessels.
Early postpartum bleedings arise in the first 2 hours after the delivery, but later ones may develop in the period from 2 hours to 6 weeks after the childbirth. The outcome of postpartum bleeding depends on the volume of the lost blood, the bleeding intensity, efficiency of the carried out conservative therapy and the development of the disseminated intravascular coagulation syndrome. Prevention of postpartum bleeding is the actual problem of obstetrics and gynecology.
Causes of Postpartum Bleeding
Postpartum bleeding often arises because of disorders of contractile myometrium function, such as hypotonia (decrease in the uterine tone and its insufficient contractile muscles activity) or atony (total loss of the tone of the uterus and its ability to contract, lack of myometrium reaction on stimulation). Such postpartum bleedings may be caused by fibromas and myomas of the uterus and cicatricial processes in myometrium. Excess stretching of the uterus at multiple pregnancy, polyhydramnios, protracted labor with a large fetus; application of the preparations reducing the uterine tone can serve as a reason to postpartum bleedings, too.
Postpartum bleeding may be caused by afterbirth remainders in the uterine cavity such as segments of the placenta and parts of fetal covers. It interferes with the normal contractile uterus functioning, provokes development of inflammations and sudden postpartum bleeding. The partial increment of the placenta, incorrect managing of the third stage of labour, uterine contractions mismatch or uterine cervix spasm could lead to anomalous expulsion of afterbirth.
As the factors provoking postpartum bleeding, the hypotrophy or an atrophy of endometrium for earlier carried out surgeries, such as Cesarean section, abortions, a conservative myomectomy, or uterus raclage can serve.
The appearance of postpartum bleeding may be promoted by haemocoagulation disorders in mother’s body caused by congenital anomalies, taking anticoagulants, or development of disseminated intravascular coagulation syndrome.
Quite often postpartum bleeding develops in traumatic injuries (as tearings) or dissections of genital tract bodies during delivery process. The high risk of postpartum bleeding arises because of gestosis, incorrect presentation and a premature abruption of placenta, threat of pregnancy termination, fetoplacentary insufficiency, pelvic presentation of the fetus, mother’s endometritis or cervicitis, cardiovascular and central nervous system chronic diseases, kidneys or liver chronic liver dysfunctions.
Symptoms of Postpartum Bleeding
The clinical manifestations of postpartum bleeding are caused by quantity and intensity of the blood loss. At the atonic uterus which isn't reacting to external medical manipulations, postpartum bleeding is, as a rule, profuse. But it also may have wavelike character, being reduced sometimes under the influence of the preparations contracting the uterus. Objectively arterial hypotonia, tachycardia, pallor of skin is observed.
Blood loss volume up to 0.5 % of body weight is regarded for a woman in labor as physiologically admissible. Further increase in the volume of lost blood implies pathological postpartum bleeding. The blood loss exceeding 1 % of body weight is considered as massive, larger amount is critical. At critical blood loss there may even be a hemorrhagic shock and disseminated intravascular coagulation syndrome with irreversible changes in vitals.
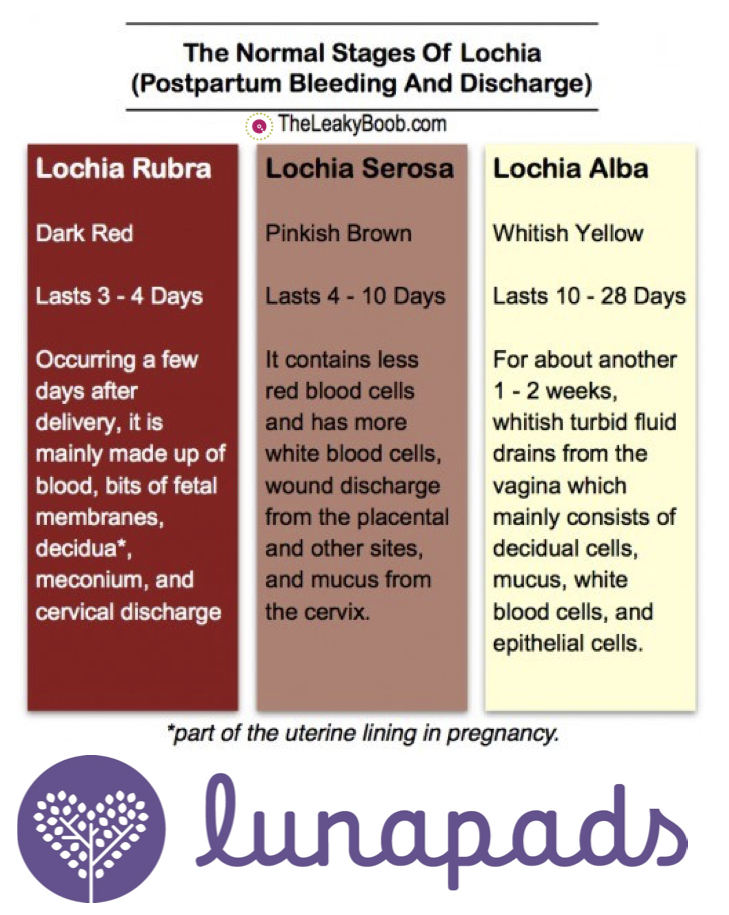
During the late postnatal period intensive and long lochia, discharge of bright red color with big clots of blood and unpleasant odour, nagging abdominal cramps must get the woman to be more cautious.
The modern clinical gynecology can carry out an assessment of the risk of postpartum bleeding which includes monitoring of blood hemoglobin level, quantity of erythrocytes and platelets in blood serum, time period of bleeding and fibrillation and a condition of the blood coagulation system (coagulogram) during pregnancy.
Hypotonia and atony of the uterus may be diagnosed during the third stage of labour by weak myometrium contractions and its flabbiness, and because of more longer placental stage.
Diagnosis of postpartum bleeding is based on careful inspection of integrity of incremented placenta and fetal covers, and also examination of maternal passages with the object of accidental injury detecting. The gynecologist carefully carries out manual research of the uterine cavity under the general anesthesia on existence or lack of tearings, remainders of afterbirth, blood clots,malformations or tumors, which hinder myometrium from contraction.
A permanent role in the prevention of late postpartum bleeding is played by ultrasonic investigation of the small pelvis bodies carried out on the 2nd and the 3rd days after the delivery allowing to find the remained fragments of placentary tissue and fetal covers in the uterine cavity.
Treatment of Postpartum Bleedings

At postpartum bleeding establishment of the reasons, elicit the conditions for the arising and prevention of intensive blood loss, restoration of the normal volume of circulating blood and stabilization of level of arterial pressure is paramount. The simplification of procedures with application as conservative (medicamentous, mechanical), and surgical methods of treatment is important to combat postpartum bleeding.
In order to stimulate the contractive activity of uterine muscles, they carry out catheterization and bladder emptying, a local hypothermia (by putting an ice-poultice on a stomach bottom), the sparing external massage of the uterus, and in the absence of result intravenous administration the uterotonic drugs (generally, it is methylergometrine with oxytocin), injections of prostaglandins to the cervix of the uterus.
For restoration of the circulating blood volume and elimination of consequences of intensive blood loss during postpartum bleeding, they carry out infusion and transfusion therapy by components of blood and plasma-substituting preparations.
In case of detection of the uterus cervix ruptures, or the vagina and perineum walls tearings during examination of maternal passages by mirrors, such ruptures are stitched under local anesthesia. The uterine cavity urgent manual examination is conducted under the general anesthesia if disruption of the placenta takes place (even in absence of bleeding), and also at hypotonic postpartum bleeding. During control of the uterine walls they carry out manual extraction of the afterbirth remainders and the placenta covers, as well as blood clots. Researches with the object to determine a presence of the uterine body ruptures are also performed.
If the uterine body ruptures have been detected, the emergency laparotomy, the sewing up of a wound or even removal of the uterus is fulfilled. At detection of signs of the placenta increment, and also at intractable intensive postpartum bleeding the uterus extirpation is required (with bandaging internal iliac artery or embolization of the uterine vessels if necessary).
Surgeries at postpartum bleeding are carried out along with resuscitation actions, such as compensation of blood loss, stabilization of haemodynamics and arterial blood pressure. Their timely realization before development of disseminated intravascular coagulation can surely rescue the woman in labor from death.
Prevention of Postpartum Bleeding
Some women with the adverse obstetric and gynecologic anamnesis, blood coagulation disorders, or the women taking anticoagulants have rather high risk of development of postpartum bleeding and therefore they ought to be under special medical care during their pregnancy period and go to specialized maternity hospitals.
In order to prevent postpartum bleeding, the preparations promoting adequate contractions of the uterus are administered to women. During the first two hours after the delivery all women who have given birth to their children, rest in maternity ward under dynamic supervision of medical personnel for assessment of the blood loss volume in the early postnatal period.
Video: What can I expect with postpartum bleeding?