Diabetes During Pregnancy
Contents:
- Dangers of the Gestational Diabetes While Pregnancy
- Difference of Other Types of Diabetes Mellitus
- Classification of Diabetes Mellitus Types
- Causes of Pregnancy Diabetes
- Risk Groups in Development of Diabetes Mellitus While Pregnancy
- Symptoms and Signs
- Treatment of Diabetes Mellitus While Pregnancy
- Nutrition (Diet) of Pregnant Diabetes Mellitus Patients
Gestational Diabetes During Pregnancy
Diabetes mellitus of pregnant women is disorder of a carbohydrate metabolism originated or diagnosed for the first time in the period of pregnancy. The degree of disturbance of exchange processes can be diverse: from "pre-diabetes" – disorders of glucose tolerance, till an emergence of an unwrapped clinical picture of the disease with its intrinsic complications. The Gestational Diabetes Mellitus is, indisputably, one of the central problems of obstetric practice.
Dangers of The Gestational Diabetes While Pregnancy
In case of presence of gestational diabetes, complications of the pregnancy are by no means rare phenomenon. The development of this disease at early terms of pregnancy is prone to sharp increase of risk of spontaneous abortion (i.e. miscarriage). Even if pregnancy is maintained, one can not exclude likelihood of a baby's having various congenital malformations, in addition, the tot`s vital organs (heart and brain) will become the first place "target" of the disease. If the disease attacks an organism of a pregnant woman on the 2nd or 3rd trimester, this can become the cause of a macrosomia (excessive mass of a fetus) and to a diabetic fetopathy after the birth.
Diabetic fetopathy is a frightful disease of the neonatal period, typical manifestations of which are the following: large mass of a newborn, disproportion of the body, big shoulders and relatively short and thin limbs, magnified abdomen in consequence of excessive increase of subcutaneous fat, swelling of the soft tissues and skin, the swelling of the face, the yellowness of skin, the presence of “punctate” hemorrhages, the disorders of respiration, glucose is lowered and viscosity is increased in blood. Some changes of the neurological status are possible: insufficient muscle tone, physiological reflexes are oppressed (sucking one), alternation of periods of inactivity and hyperexcitability.
Difference of Other Types of Diabetes Mellitus
Diabetes mellitus is the frightful endocrine-metabolic disease, the cause of which is a shortage and/or inefficiency of insulin hormone (it is synthesized by the pancreas) characterized by pathology of the metabolism (in the first place, of the carbohydrate one). Almost always hyperglycemia (sugar fasting blood level increased above physiological normal condition) and glucosuria (presence of the glucose in urine) are laboratory criteria of this diagnosis establishing.
Classification of Diabetes Mellitus Types

The diabetes mellitus is classified as follows.
- The type 1 diabetes (insulin-dependent one) arises as a result of an injury or decay of cells secreting insulin (special cells of a pancreas), which leads to the sharp decrease or complete discontinuation of its production. Often autoimmune aggression underlies this pathology. As a rule, in this case the debut of a clinical manifestation occurs in the child (or more rarely – young) age. The number of the ones suffering from the type 1 diabetes is about 15-20 % from the total amount of patients. The diagnosis is made during a revelation of inexplicably high level of blood glucose in the young age and/or detection of specific antibodies against cells of the pancreas. The rates of insulin in blood of these patients are always decreased. For maintenance of normal range of blood glucose, retention the diseases in the compensation state and prevention of complications, insulin injections are vitally important.
- The diabetes mellitus type II (insulin-independent one) develops in consequence of defect of insulin secretion. The insulin resistance (non-susceptibility of an organism to insulin) is the important factor. About 80-85 % of diabetics suffer exactly from this type of diabetes. Elderly people are susceptible to the disease more often. "Risk groups" include: people with excessive body mass, chronic or acute pancreatitis patients. A previous infectious disease, an intake of some drugs, effect on an organism of chemical substances can become the impetus to development of the disease. The defining role is assigned to genetic predisposition. Hyperglycemia serves as the key laboratory sign of the disease. The therapy of such patients includes special diet compliance, dosed physical activities, the intake of special drugs (antihyperglycemic peroral remedies).
Causes of Pregnancy Diabetes
The decreased non-resistance of an organism, i.e. its cells and tissues, to its own hormone insulin (insulin resistance) underlies this disease. Its development is linked mainly to the rise in blood of the level of hormones, typical to the pregnancy period. In addition, the glucose requirement of the fetus is sufficiently high, which leads to increased consumption of the glucose by the placenta and sharp reduction of the level of glucose in blood of the pregnant woman. The organism tries to "compensate" the low content of glucose and stimulates the pancreas to intensely secrete insulin. Gradually, the reserves of the pancreas become exhausted, it loses ability to produce insulin in the needed amount, thus, conditions for pregnancy diabetes are created.
It is the fact, that after the labor the indicators of glucose return to the normal values sometimes. However, even then, one can not completely exclude a possibility of development of the disease. One needs to necessarily give attention to the diabetes prophylaxis. 10-14 weeks after the child birth, the repeat testing for diabetes is recommended. If survey does not reveal deviations – continue to be checked at least once in 3 years. It is desirable to also undergo survey for the level of glycated hemoglobin.
Risk Groups in Development of Diabetes Mellitus While Pregnancy
The significant role in development of this disease belongs to hereditary predisposition.
The launch factors for its implementation can be the following:
- excesses weight, presence of obesity;
- the age of a woman over 30 years;
- presence of other disorders of the carbohydrate metabolism;
- glucose runs with urine (in vitro);
- diabetes mellitus of relatives (especially, of the closest ones);
- arterial hypertension and another cardiovascular pathology;
- presence in an of toxicosis, gestosis in the anamnesis;
- polyhydramnios;
- dead birth or cases of miscarriage in the previous pregnancies;
- congenital pathology of other children in the family;
- gestational diabetes in the previous pregnancies.
Diabetes Mellitus While Pregnancy: Symptoms and Signs
This disease does not have any specific manifestations. One can often make a diagnosis only by means of pregnant woman screening. The women belonging to risk groups should certainly check indicators of fasting blood sugar. If this indicator exceeds the norm, the woman must undergo "the load test with glucose". For the purpose of the revelation of the GDM (Gestational Diabetes Mellitus), on the term of 6-7 months, all the pregnant women are exposed to conducting of a glucose tolerance test reflecting the quality of assimilation of glucose by an organism.
If the test results exceed normal condition, the physician has strong reasons to make the GDM diagnosis. Repeated conducting of the test is possible (in a case need). If the diagnosis is made in time and the woman is under observation of specialists (endocrinologist and gynecologist obstetrician), strictly observing all their recommendations, the risk of a sick baby birth reduces enormously.
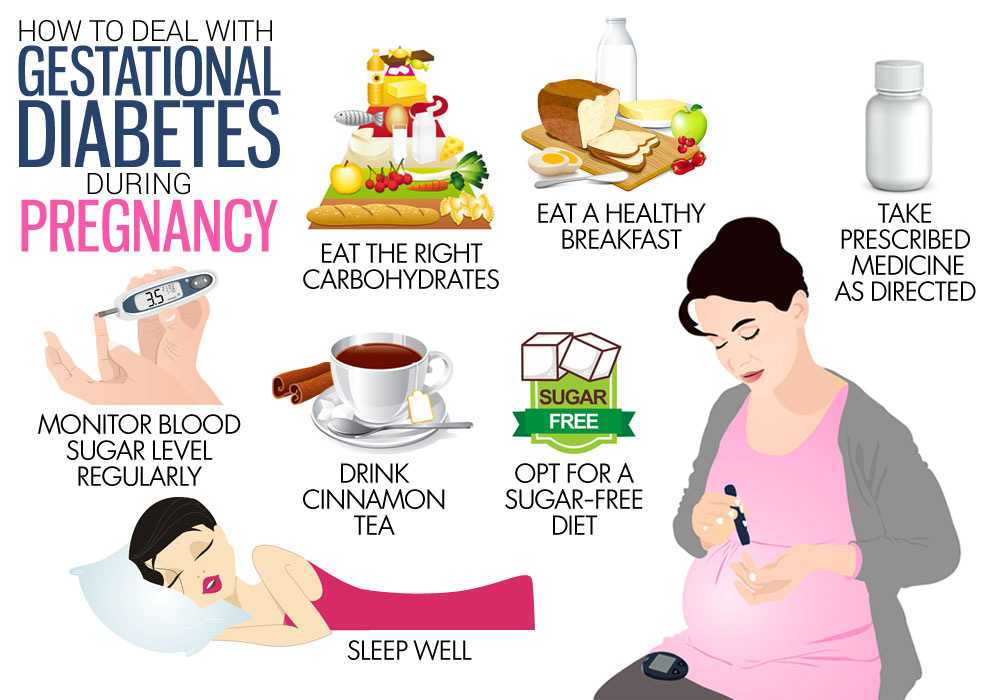
Treatment of Diabetes Mellitus While Pregnancy
The woman needs to constantly control rates of blood glucose (+ at a minimum, 4 times a day). Dietary intervention is necessary for adjustment of the disease. The day amount of calories is to be limited up to 25-30 per 1 kg of weight. The fetal development directly depends on meals. The intake of antihyperglycemic drug is strictly contraindicated in the period of pregnancy. If the diet and the moderate physical activity do not produce the due effect, one needs to opt for the insulin therapeutics.
Nutrition (Diet) of Pregnant Diabetes Mellitus Patients
The correct meals are an integral component of successful treatment. One needs to focus attention on reduction of calorific food value, in no way affecting its nutritional value.
The following simple recommendations are developed by the physicians:
- always take meals by small serves and only in the same time;
- except products containing easily digested carbohydrates from the menu (pastries, bananas, biscuit, cakes, candies, figs);
- categorically refuse fatty dishes, fried dishes and food of immediate cooking;
- to the maximum enrich the diet by various paps (buckwheat, rice, peeled, wheat or pearl barley grains), vegetable and fruit salads (i.e. food with abundant content of cellulose);
- eat meat of non-fat kinds, fish and poultry;
- increase the intake of liquid (the minimum is 1,5 liters a day).